LDN Treatment Helps to Kill Cancer Cells

According to a report in The International Journal of Oncology, giving low dose naltrexone (LDN) to cancer patients can improve the immune system’s ability to kill cancerous cells, as well as improve the efficacy of standard cancer treatments and immunotherapy.
This major breakthrough gives research credence to what some doctors have observed in their cancer patients for years, and which was detailed in this short film The Game Changer produced for the LDN Research Trust.
The video includes extensive interviews with doctors who have prescribed LDN for cancer patients, as well as researchers, patients, and a pharmacist. You can find it at the bottom of this post.
In the video, Dr. Dana Flavin, of the CollMed Foundation, had this to say of LDN’s impact on immune systems: “Any of my cancer patients who have cancer should be on low-dose naltrexone because it is helpful for them in every area of cancer therapy – period,” Flavin said.
“If I had [cancer] myself, I would be on low-dose naltrexone and I’m a physician. And a pharmacologist. And a former FDA official. And I would recommend it to any and every one of my patients. It is imperative as far as I’m concerned as a support measure and we need to realize this.”
Flavin notes, as does the research, that LDN is not itself a “cure” but when used in conjunction with other treatments can help to keep people survive cancer and remain in remission.
The following is an excerpt from The LDN Book, chapter by Dr. Angus G. Dagleish with Dr. Wai M. Liu. It has been adapted for the web.
Can LDN Treatment Kill Cancer Cells?
As of this book’s publication, there have been only two controlled clinical trials on low dose naltrexone (LDN) and the treatment of cancer: one on breast cancer, which was terminated because of poor accrual, and one on glioma, which has finished but is yet to be reported on.
Most of the clinical data with regard to cancer is therefore anecdotal or small series. A pioneer of the exploration of the use of LDN in treating numerous different conditions was Dr. Bihari, who as of March 2014 was reported as having treated 354 patients.
According to the LDN website, he claimed an objective response of approximately 20% and stabilization in approximately 25%.
If these were the results of a rigorous randomized trial, without other treatments, they would be most impressive, even by the standards of the newer, more active candidates of today.
I was fortunate to visit the clinic once and to have read numerous anecdotes, but I felt at the time that the data included too many other co-treatments to justify the claims about LDN.
However, in 2002 an oncologist and an assistant from the National Cancer Institute reviewed thirty charts from Dr. Bihari’s office, of which half were chosen as appearing, without question, to have responded to LDN, confirming that there are several anecdotes where LDN appears to be the only major therapy that has led to clinical responses or long-term stabilization of the disease.
What is remarkable is that LDN’s efficacy is not confined to any single tumor type, but involves melanoma, lung cancer, pancreatic cancer, renal cell cancer, prostate cancer, and lymphomas, among others.1
My own personal experience [AGD] with LDN treatment has included high-risk patients with multiple liver metastases who have failed standard chemotherapy, which has led to both long-term disease-free status and long-term stable disease.
I also believe LDN has contributed to stabilization of aggressive disease in patients who have had tumor types other than melanoma, including advanced ovarian cancer and advanced prostate cancer.
In addition, two patients who had both progressed through standard treatment for stage IV glioma had remarkable stabilization on LDN for six months, having progressed even during standard radiotherapy and chemotherapy.
However, it was the appearance of marked whole body vitiligo in a melanoma patient who started on LDN that raised the question of an alternative mode of action.
He had progressed following a disease-free period of nearly four years, on an immunotherapy program given for nonresectable recurrence of a melanoma in the head and neck involving the neck lymph nodes.
Upon recurrence of his pulmonary metastases, he was commenced on LDN and within one week developed severe whole body vitiligo, which is a feature consistent with activated cytotoxic T cells recognizing tyrosinase.
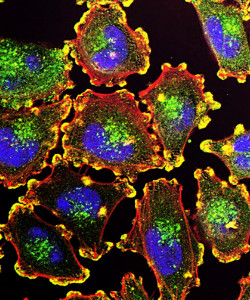
Anti-Cancer Properties of Naltrexone
It has been shown, mainly through the work of Dr. [Ian] Zagon, that low doses of naltrexone are capable of suppressing tumor growth.2
A definitive mechanism of action has yet to be established, but the effect could be achieved through direct antagonism of tumor growth or via modifications to the host immune system.
Tumor outcome is a balance of growth and death, and naltrexone—as well as other opiates and opiate antagonists—is capable of altering this balance.
In addition to their universally accepted analgesic qualities, opioids have also been reported to elicit a number of other cellular responses that lead to tumor death.
The diversity of these effects has made it difficult to establish a major cause, and serves only to confound the identification of the principal mechanism of action.
Indeed, they include those that are pro-survival in nature such as the induction of proliferation and protection against cell death, as well as polar opposite effects, including growth inhibition and the induction of apoptosis.
The ultimate consequences of treatment with naltrexone are determined by dose and schedule. Nevertheless, studies exist to try to best delineate the action of the opioids and their cognate receptors, and in doing so design new therapeutic strategies to best utilize this fascinating class of compound.
 In the early 1960s, it was reported that morphine possessed the capacity to disrupt the normal physiology of tumor-bearing rats.3
In the early 1960s, it was reported that morphine possessed the capacity to disrupt the normal physiology of tumor-bearing rats.3
The study was undertaken primarily to explore the appetite-disruptive nature of morphine on animals with tumors.
However, in addition to showing that morphine could reduce the weights of these animals, the study also showed that tumor weights were concomitantly increased in those mice given morphine.
The reason for this increase in tumor size was unclear, but it was perceivable that morphine could have secondary effects on the immune system, rendering the host more favorable to cancer growth.
Indeed, morphine has been shown to be immunomodulatory in some instances, and thus it can alter the quality of the adaptive immune response.4
Alternatively, the increase in tumor size could simply have been due to a direct effect of morphine that resulted in enhanced cellular proliferation or in reduced cell death.
The induction of apoptosis is a biological necessity and forms parts of embryonic development and normal homeostasis, and as such, disruptions can lead to a variety of diseases and disorders.5
Morphine has been shown to singly prevent both normal and desired cell death in the ciliary ganglion of the chick embryo, suggesting that in addition to modulating neurotransmission, morphine and other endogenous opiates may regulate neurophysiology.6
In this case, the concentration of morphine appeared to be important, as apoptosis was only disrupted when used at higher doses; no effect was seen at lower doses.
The importance of concentration was corroborated by another study, this time on rats, which showed higher morphine concentrations (25–200 micromolar [μM]) were able to protect primary rat neonatal astrocytes from apoptosis induced by nitric oxide.7
In this study, it was also noted that the mechanism involved, in part, modulation of the PI3-kinase (PI3-K) cascade.
This opened the doors to the possibility that morphine and other opioids might be able to influence the growth and survival of cancer cells. This was indeed the case, and a number of review articles have summarized the influences that morphine has on tumor fate.8
Unfortunately, the literature is still unclear and in many cases is contradictory.
Reports simultaneously show that morphine is able to inhibit the growth of cancer cells as well as stimulate their growth in vitro.
The cancer cells studied have been varied, representing virtually all cancer types, and all have been shown to be responsive. As some of these cancer cell lines express relatively low levels of the opioid receptors,9 one suspects the effects may be both dependent and independent of these receptors.
Furthermore, as both pro- and anti-cancer effects were seen in animal models, it has been postulated that the impact of morphine on the immune system is also likely to determine tumor fate.10
However, the conclusions of a recent review added to the confusion by saying the evidence of an effect on anti-tumor immunity was inconclusive.11
The effect of morphine on angiogenesis also cannot be discounted12 and only reinforces the view that in addition to receptor-dependent mechanisms, opioids may influence cellular fate in other ways.
LDN As An Anti-Cancer Agent
There is a good scientific reason to take LDN seriously as having a potential role as an anti-cancer agent.
First, it is an anti-inflammatory, a class of agents that have been proven to improve cancer outcomes as shown by numerous aspirin and COX-2 inhibitor studies as well as the surprising benefit reported with statins.
Second, LDN appears to have a marked immune modulatory response leading to an increase in innate immunity (such as natural killer cell activity) with a possible knock-on effect on CD8 adaptive T cells (the appearance of vitiligo after commencing LDN can only be explained by the induction of CD8 cells against tyrosinase).

Third, cancer patients can be suppressed by their disease, its treatments, and the psychological effects of living with a lethal condition.
Patients report a remarkable benefit from commencing LDN with regard to their psychological status, feeling much better than on previous treatments, which may be due to its subtle effects on various opiate receptors.
Future research must focus on LDN’s role as an additive agent with other treatments, as it can be added to most other treatments (with the exception of opiates) and, in the case of oncology, it appears to enhance the effects of some other treatments such as platinum.
There is a very high chance that it will be most effective in some subtle combination.
It is already sold with alpha lipoic acid and has been reported to be enhanced by the addition of metencephalin or OGF. However, the true benefit of these combinations remains to be shown in clinical trials.
Some combinations make perfect sense, such as making sure the recipient is vitamin D3 replete.
Low vitamin D levels have been suggested as a major cause for nonresponse to LDN in multiple sclerosis patients, and low levels of vitamin D greatly reduce the efficacy of anti-tuberculosis chemotherapy and melanoma treatment.
Mechanisms of action discussed previously strongly suggest benefit potential with immunotherapy such as vaccines, cytokines, and possibly checkpoint inhibitors. Similarities already mentioned suggest a great potential in combining LDN with the cannabinoids, to name but one example.
In summary, there are many reasons for developing LDN as an anti-cancer agent either as an adjuvant or in combination with other agents.
Unfortunately, the numerous anecdotes currently reported still require confirmation with properly conducted clinical trials, which are very expensive.
The cost of clinical trials is the major reason why they have not been done to date, as the intellectual property, based on current patent filings (over 350), is not strong enough to protect development.
It is hoped that this can be addressed in the near future and that LDN can achieve a license for adjuvant use in cancer management.
Watch
“The Game Changer” – LDN & Cancer from LDN Research Trust on Vimeo.
Notes
- B. M. Berkson et al., “Revisiting the ALA/N (Alpha-Lipoic Acid/Low-Dose Naltrexone) Protocol for People with Metastatic and Nonmetastatic Pancreatic Cancer: A Report of 3 New Cases,” Integrative Cancer Therapies 8, no. 4 (December 2009): 416–422; and B. M. Berkson et al., “Reversal of Signs and Symptoms of a B-Cell Lymphoma in a Patient Using Only Low-Dose Naltrexone,” Integrative Cancer Therapies 6, no. 3 (September 2007): 293–296.
- I. S. Zagon and P. J. McLaughlin, “Naltrexone Modulates Tumor Response in Mice with Neuroblastoma,” Science 221, no. 4611 (August 1983): 671–673.
- H. Sobel and G. Bonorris, “Effect of Morphine on Rats Bearing Walker Carcinosarcoma 256,” Nature 196 (December 1962): 896–897.
- P. Sacerdote, “Opioids and the Immune System,” Palliative Medicine 20 (January 2006): 9–15.
- S. Elmore, “Apoptosis: A Review of Programmed Cell Death,” Toxicologic Pathology 35, no. 4 (2007): 495–516.
- S. D. Meriney et al., “Morphine-Induced Delay of Normal Cell Death in the Avian Ciliary Ganglion,” Science 228, no. 4706 (June 1985): 1451–1453.
- M. S. Kim, “Protective Effects of Morphine in Peroxynitrite-Induced Apoptosis of Primary Rat Neonatal Astrocytes: Potential Involvement of G Protein and Phosphatidylinositol 3-Kinase (PI3 Kinase),” Biochemical Pharmacology 67, no. 7 (April 2001): 779–786.
- I. Tegeder and G. Geisslinger, “Opioids as Modulators of Cell Death and Survival—Unravelling Mechanisms and Revealing New Indications,” Pharmacological Reviews 56, no. 3 (September 2004): 351–369; B. Afsharimani et al., “Morphine and Tumor Growth and Metastasis,” Cancer and Metastasis Reviews 30, no. 2 (June 2011): 225–238; K. Gach et al., “The Role of Morphine in Regulation of Cancer Cell Growth,” Naunyn-Schmiedeberg’s Archives of Pharmacology 384, no. 3 (September 2011): 221–230; and S. Bimonte et al., “The Role of Morphine in Animal Models of Human Cancer: Does Morphine Promote or Inhibit the Tumor Growth?,” BioMed Research International (2013): 1–4.
- K. Gach et al., “Opioid-Receptor Gene Expression and Localization in Cancer Cells,” Central European Journal of Biology 6, no. 1 (February 2011): 10–15.
- M. Ishikawa et al., “Enhancement of Tumor Growth by Morphine and Its Possible Mechanism in Mice,” Biological & Pharmaceutical Bulletin 16, no. 8 (August 1993): 762–766.
- J. W. Boland, “Effects of Opioids on Immunologic Parameters That Are Relevant to Anti-tumour Immune Potential in Patients with Cancer: A Systematic Literature Review,” British Journal of Cancer 111, no. 5 (August 2014): 866–873.
- L. Koodie et al., “Morphine Inhibits Migration of Tumor-Infiltrating Leukocytes and Suppresses Angiogenesis Associated with Tumor Growth in Mice,” The American Journal of Pathology 184, no. 4 (April 2014): 1073–1084.
Recommended Reads
Treating Addiction: From Opium Poppy to Morphine to Naltrexone
Recent Articles
Asparagus is a delicious vegetable with a layered history. How did this aspiring spear make its way from growing in the wild to appearing on our plates? The following is an excerpt from the The Seed Detective by Adam Alexander. It has been adapted for the web. “Nature gives us the key to every secret…
Read MoreChances are, you’ve seen cattails growing on the edge of your local lake or stream at least once or twice. Instead of just passing these plants, try foraging for and cooking them to create delicious seasonal dishes! The following excerpt is from The New Wildcrafted Cuisine by Pascal Baudar. It has been adapted for the…
Read MoreGarlic mustard: while known as “invasive,” this plant can be consumed in its entirety and has great nutritional value. Plus, the garlic-flavor is a perfect addition to any recipe that calls for mustard! The following are excerpts from Beyond the War on Invasive Species by Tao Orion and The Wild Wisdom of Weeds by Katrina…
Read MorePeregrine falcons, while known as predators, are essential to our environment. These stunning birds have a rich history, an interesting present, and an uncertain future. The following is an excerpt from Feather Trails by Sophie A. H. Osborn. It has been adapted for the web. Who Are Peregrine Falcons? Though relatively uncommon wherever it occurs,…
Read MoreMany know the effects of catnip on our feline friends, but few realize that catnip has medicinal effects for humans. From stomach aches to reducing fevers, catnip is a versatile herb with many benefits. The next time you grow this plant for your cat you may end up taking a few cuttings for yourself! The…
Read More